Prostatitis is a common urological disease that can occur in any man over the age of 30, and every year the probability of its development only increases. This disease causes serious male problems: acute prostatitis leads to depression, decreased libido and, in general, disorders of the genitourinary system; chronic condition causes diseases of the urological sphere, infertility, impotence.
general information
Prostatitis is an inflammatory lesion of the prostate, an organ that only men have. Iron makes three most important functions:
most important functions:
- secretory - produces a special enzyme that regulates sperm viscosity and ensures the viability of male germ cells for successful egg fertilization;
- motor - controls the muscle tissue of the urethral sphincter, due to which the proper process of urine outflow occurs, and the secretion of the prostate is released during ejaculation;
- barrier - prevents the penetration of infectious agents into the upper urinary tract from the urethra, provides an antibacterial barrier, as part of the male immune system.
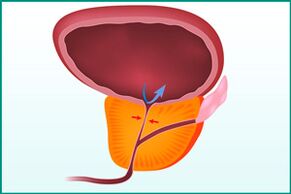
In prostatitis, the prostate enlarges and begins to squeeze the urethra, which disrupts the normal flow of urine. The organ itself is unable to fully perform its functions due to inflammation.
Reasons
The source of men's health problems - prostatitis - can develop for the following reasons:
- Presence of congestion in the pelvic area. Most often, such blood stagnation occurs due to a sedentary, immobile lifestyle and excess weight.
- Infectious infection of the prostate. It can be descending (via urine) or ascending (through the urethra), entering the prostate together with blood or lymph.
The development of prostatitis usually occurs against the background of the presence of certain risk factors:
- lack of physical activity;
- maintaining a sedentary lifestyle;
- irregular sex life;
- hypothermia, especially covering the pelvis;
- the presence of injuries in the pelvic area;
- weakened immunity;
- malnutrition with an abundance of sweet, fatty and fried foods;
- the presence of bad habits;
- infection with sexually transmitted infections.
Species
According to ICD-10 (International Classification of Diseases), there are 4 types of prostatitis:
- Acute prostatitis.
- Chronic bacterial prostatitis.
- Chronic prostatitis is non-bacterial, inflammatory and non-inflammatory.
- Chronic prostatitis, asymptomatic.
In the acute form of the disease, the symptoms appear strongly and clearly, the inflammatory process develops rapidly. The usual causes are infection of the prostate by infectious agents that penetrate from the urethra or blood.
Chronic bacterial form - acute prostatitis, which was not cured in time. The same factors that affect acute inflammation contribute to the development of the pathological condition - infections of the genitourinary system and blood stagnation in the pelvic organs.
Nonbacterial chronic prostatitis (also called chronic pelvic pain syndrome) is most commonly found in older men. It can also develop against the background of impaired prostate function and as a result of the body's autoimmune reaction.
Chronic asymptomatic prostatitis is an inflammation of the prostate, during which patients do not experience any unpleasant sensations.
Clinic
The clinical picture of acute prostatitis has very vivid manifestations that cannot be ignored and are very difficult to live with:
- increase in body temperature over 38 ° C;
- chills with sweat and weakness;
- severe pain in the lower abdomen, perineum, genitals;
- urination disorder - difficulty, pain, acute retention of urine.
In the case of chronic prostatitis, there are similar, but less pronounced symptoms that are often ignored:
- dull aching pain in the perineum and lower abdomen, radiating to the sacrum and genitals;
- difficult urination, painful and accelerated with imperative (sharp and irresistible) urges, most often at night;
- erectile dysfunction;
- decrease in the quality and duration of sexual intercourse;
- reduction in the difficulty of orgasm.
Asymptomatic course of prostatitis proceeds without complaints from the patient. The problem is discovered incidentally during prostate and/or urine tests.
Diagnostic methods
If prostatitis is suspected, the doctor conducts a diagnosis, the first step of which is to clarify complaints and study the anamnesis. Information is collected on all symptoms and their development. Following are the activities:

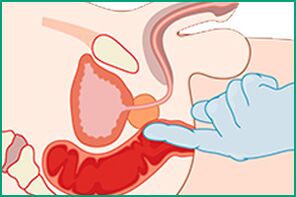
- Palpation of the prostate through the rectum to determine the size of the organ, its density and pain. For further bacteriological analysis in the probing process, the secret of the gland is also collected. The purpose of the study is to rule out a number of diagnoses: prostate adenoma or cancer, rectal cancer.
- Ultrasound and TRUS to supplement and clarify data obtained during palpation.
- Bacteriological analysis of prostate secretions to detect infection and determine the type of pathogen. The data is needed to select and prescribe antibiotics.
- A blood test to determine the level of PSA (prostate-specific antigen) - allows you to rule out adenoma and gland cancer.
- Biopsy - examination of a sample of prostate tissue under a microscope to confirm or deny adenomas and cancer.
Treatment
Modern urology considers three types of treatment for acute prostatitis and exacerbations of the chronic form of the disease:
- medicines;
- surgical;
- physiotherapy.
Drug exposure includes taking penicillin, fluoroquinolone, macrolide, tetracycline, cephalosporin, or aminoglycoside antibiotics. A certain medicine is prescribed by the doctor, depending on which infectious agent caused the inflammation. In addition, patients are prescribed:
- anti-inflammatory drugs to eliminate fever;
- pain relievers;
- antispasmodics to normalize urine output;
- alpha blockers to relieve symptoms and restore healthy urination.
In the absence of drug effect or in advanced cases of acute prostatitis, the doctor may prescribe a surgical intervention, during which the entire prostate or part of it is removed. Surgery is necessary for patients with accompanying complaints: stones in the prostate or neoplasms of a benign and malignant nature.
Physiotherapy is an addition to medical treatment, it can be done only after the acute inflammatory process has been eliminated. Patients are shown:
- massage;
- exercise therapy (physiotherapy);
- magnetotherapy;
- ultrasound treatment;
- electrical stimulation;
- microwave and laser exposure;
- reflexology.
Appointment of a certain type of procedure is performed by the attending physician.
With chronic prostatitis during remission, the patient must:
- undergo regular examinations and, if necessary, a course of antibiotic therapy;
- eat properly, avoiding exhaustion and excess weight;
- protect the body from hypothermia;
- engage in exercise therapy, and the exercises should strengthen the muscles of the lower abdomen and pelvic floor;
- have a regular sex life;
- get rid of bad habits.
Prostate massage is also a useful procedure, which improves circulation and the outflow of secretions in the organ, and this helps prevent the recurrence of the acute stage of the disease.
Complications
Complications of prostatitis manifest both in the prostate itself and in the organs surrounding it, which is due to the anatomical location. In an acute form, infectious agents can reach the bladder and kidneys, inflammation - to the fatty tissue of the gland, venous plexus and rectum.
Chronic disease is dangerous because it affects not only the tissues and organs surrounding the prostate, but also the nervous, urological and reproductive areas.
Possible complications of acute prostatitis:
- abscess;
- phlebitis of venous plexuses in the small pelvis;
- inflammation of fatty tissue;
- orchitis;
- epididymitis;
- vesiculitis;
- pyelonephritis.
Chronic prostatitis causes the following complications:
- chronic pain syndrome;
- sexual dysfunction;
- infertility;
- violation of the urination process;
- general deterioration of the quality of life.
impotence and infertility
The two most common problems associated with prostatitis are impotence and infertility. The development of each condition occurs against the background of chronic prostate damage.
Impotence (erectile dysfunction) is manifested in 40% of cases of neglected and untreated prostatitis. The development of complications occurs over a long period of time, sometimes even years. His reasons:
- violation of the prostate with the wrong passage of nerve impulses and failure of hormone production;
- deterioration of control over the pelvic muscles responsible for the occurrence of an erection;
- psychological insecurity;
- pain syndrome, which causes fear of possible failure in bed.
It is impossible to talk about the unconditional connection of prostatitis with infertility. This disease has an indirect effect on a man's reproductive capacity and only with an advanced chronic course. Causes of fertility problems in the background of prostate damage:
- decrease in the quality of seminal fluid;
- decrease in the number and mobility of spermatozoa;
- the presence of germ cell damage and defects;
- vas deferens scars;
- failure of secretory function;
- testicular dysfunction.
In acute prostatitis, spermatozoa are damaged, their quality and motility deteriorate, defects occur, and a smaller number of male germ cells are created.
Prevention
Prostatitis can be prevented, but it is necessary to constantly follow a series of preventive recommendations:
- lead a healthy lifestyle with proper nutrition, reasonable physical and sexual activity and the absence of bad habits;
- engage in physiotherapy exercises aimed at removing congestion in the pelvic organs and strengthening the pelvic muscles;
- undergo examinations by urologists and andrologists in a timely manner;
- beware of hypothermia.
Prostatitis is a serious disease of the urological sphere that can cause significant damage to the male body. It is very important to pay attention to the first signs of its appearance and visit a specialist who will prescribe a complete treatment. Without it, the acute condition can become chronic and cause even greater health problems.























